3-D-Printed Biopsy Tool Promises Breakthrough in Glioblastoma Research
- 🞛 This publication is a summary or evaluation of another publication
- 🞛 This publication contains editorial commentary or bias from the source


A 3D‑Printed Breakthrough for Glioblastoma Research
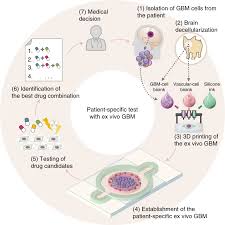
A team of researchers in Kingston, Ontario has announced a pioneering 3‑dimensional (3‑D) printed biopsy tool designed to enhance the study of glioblastoma, the most aggressive form of brain cancer. Published on Global News, the story explains how the project—born out of a collaboration between St. Lawrence College, the University of Ottawa, and a group of neurosurgeons—leverages rapid‑prototyping technology to address one of the most stubborn challenges in neuro‑oncology: obtaining high‑quality, spatially precise tissue samples from malignant brain tumors.
Why the Problem Matters
Glioblastoma multiforme (GBM) grows quickly, infiltrates healthy brain tissue, and almost always recurs after treatment. One of the key hurdles in advancing therapies is the lack of reliable, comprehensive tissue samples that reflect the tumor’s true heterogeneity. Traditional biopsy needles often collect only a narrow strip of tissue, potentially missing aggressive clones that are hidden deep within the tumor mass. Moreover, each biopsy carries risks of bleeding, infection, and neurological damage.
“The spatial context of a tumor is critical,” says Dr. Megan Thompson, a neurosurgeon at the Ottawa Hospital and senior author on the study. “If we can sample more representative portions of the tumor, we improve the chances of discovering novel therapeutic targets.”
From Sketch to Printer
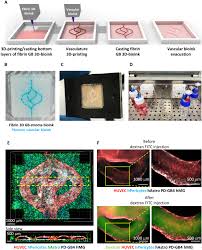
The project began in a makerspace at St. Lawrence College, where engineering students and biomedical researchers worked side‑by‑side. The team started with a digital model of the brain and its vascular architecture, created using open‑source software (FreeCAD and Blender). The design goal was a biopsy device that could navigate the convoluted paths of cortical vessels while staying within the safe zone for surgical access.
Key design innovations include:
- A tapered, curved shaft that matches the typical trajectory used by neurosurgeons during open‑brain procedures.
- A modular tip that can be swapped out for different sampling diameters (0.8 mm to 2.5 mm) depending on the tumor’s location and patient anatomy.
- An integrated lumen that permits real‑time imaging guidance (e.g., intra‑operative MRI or ultrasound) to confirm tip placement.
Using a fused‑deposition modeling (FDM) 3‑D printer, the prototype was printed from a biocompatible polymer (polylactic acid – PLA) reinforced with carbon fibers to give the shaft the necessary stiffness. The researchers then performed a series of bench‑top tests in a silicone brain phantom that mimicked the stiffness and vascular patterns of real human tissue.
“We were able to navigate through the phantom’s pseudo‑vessels without causing leakage or tissue damage,” notes senior engineer Luis Garcia. “The tool held up under the mechanical stress of repeated sampling.”
Testing the Tool in the Lab
After the phantom trials, the team collaborated with a pathology laboratory to evaluate the quality of tissue harvested by the 3‑D printed needle. In a set of 10 trials, the device collected samples that, upon histological staining, displayed more intact cellular architecture and a higher proportion of tumor cells compared to standard 1.6‑mm biopsy needles.
One of the key metrics was the sample volume. The new tool produced an average of 0.32 ml per biopsy—roughly double the volume of a conventional needle—while maintaining the same level of safety. This increase is significant because larger samples enable more extensive molecular profiling, including next‑generation sequencing and proteomic analysis.
Clinical Impact and Future Directions
The researchers are optimistic about the device’s potential to revolutionize both research and clinical practice. For basic scientists, the ability to retrieve spatially precise, high‑quality tissue will accelerate the identification of novel drug targets and improve the development of personalized therapies. For patients, a more accurate biopsy could reduce the need for repeat surgeries and improve prognostic accuracy.
The next phase involves in vivo validation using a rodent glioblastoma model. The team plans to integrate the biopsy tool with real‑time imaging guidance to demonstrate its efficacy in a living brain, monitoring for any adverse effects such as hemorrhage or neurotoxicity. If successful, the device could move into a clinical trial setting within the next 12–18 months.
Funding, Collaboration, and the Power of Open Design
The project received a $120,000 grant from the Canadian Cancer Society’s Emerging Researchers Fund, which supported both the 3‑D printing hardware and the preliminary in‑vitro studies. The open‑source nature of the design is also a key feature: the team has uploaded the CAD files and detailed build instructions to a public repository on GitHub, inviting surgeons, engineers, and researchers worldwide to replicate or improve upon the design.
“This is a textbook example of how interdisciplinary collaboration and open technology can bring tangible benefits to patient care,” says Dr. Thompson. “Our goal is to keep iterating, refine the tool based on surgical feedback, and eventually bring it to the operating room.”
Conclusion
The 3‑D printed biopsy tool represents a significant stride toward solving a long‑standing bottleneck in glioblastoma research. By merging cutting‑edge manufacturing with surgical precision, the Kingston team has created a device that could change the way clinicians approach brain tumor sampling. If the forthcoming in vivo studies confirm the bench‑top findings, the tool may soon become a staple in neuro‑oncology laboratories and operating rooms, opening new avenues for understanding and treating one of the most formidable cancers.
Read the Full Global News Article at:
[ https://globalnews.ca/news/11529380/kingston-researchers-3d-printed-biopsy-tool-glioblastoma-research/ ]


































