How a woman's journey with lupus reflects science's way of tackling the disease
- 🞛 This publication is a summary or evaluation of another publication
- 🞛 This publication contains editorial commentary or bias from the source

From Frightening Diagnosis to Hopeful Treatment: A Woman’s Journey Through Lupus Reflects the Science Behind the Disease
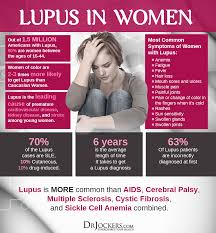
When 32‑year‑old Maria Ramirez first noticed a rash on her cheeks that spread to her nose and ears, she thought it was just a sunburn or a seasonal allergy. Within a month, she was dealing with severe joint pain, persistent fever, and a throbbing headache that didn’t respond to over‑the‑counter medication. By the time she reached a general practitioner, she was in the midst of a night‑long fever and a rash that seemed to flare up with every step she took. It wasn’t until her fourth visit to a different internist that a routine blood test revealed a red flag: a high titer of antinuclear antibodies (ANA). A specialist in rheumatology was called in, and the diagnosis was made—systemic lupus erythematosus (SLE).
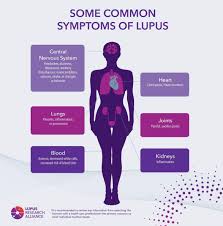
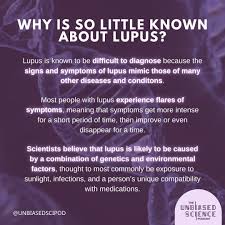
Lupus is an autoimmune disorder in which the immune system mistakenly attacks healthy tissues. Although the exact cause remains elusive, scientists know that a combination of genetic predisposition and environmental triggers—such as infections or ultraviolet light—can set the disease in motion. In Maria’s case, her family history of autoimmune disease, coupled with a recent viral infection, may have acted as a catalyst.
The Diagnostic Odyssey
Maria’s early symptoms were nonspecific, a hallmark challenge for lupus patients. “I was constantly told it was stress or a viral infection,” she recalled. “It wasn’t until the blood work showed ANA positivity that the doctor took me seriously.”
The rheumatologist ran a battery of tests—anti‑dsDNA, complement levels (C3 and C4), and kidney function panels—to confirm the diagnosis. The low complement levels and rising anti‑dsDNA titers hinted at a potential kidney involvement, a serious complication known as lupus nephritis. Early detection of these changes is crucial because untreated lupus nephritis can lead to irreversible kidney damage.
“Early intervention changes the trajectory,” the rheumatologist explained. “We want to keep the kidneys from being hit hard.”
From Pills to Personalized Medicine
Maria’s initial treatment regimen involved hydroxychloroquine, a disease‑modifying antimalarial that has become a cornerstone of lupus therapy. The drug helps reduce flares and improves skin and joint symptoms. To manage her severe pain and swelling, the rheumatologist prescribed a short course of prednisone. However, the steroid’s side effects—including weight gain, mood swings, and increased blood sugar—became a daily battle.
“Finding the right balance between controlling the disease and minimizing side effects is like walking a tightrope,” Maria noted. Her rheumatologist then introduced her to belimumab (Benlysta), a monoclonal antibody that targets the B‑cell activating factor (BAFF). This biologic agent directly attacks the abnormal B cells that produce the damaging autoantibodies in lupus.
After six months on belimumab, Maria’s joint pain decreased by 60%, and her fatigue improved markedly. She also reported fewer hospital visits, an outcome that the rheumatology team attributes to early biologic intervention—a strategy increasingly supported by recent research.
The Science Behind the Treatment
The development of belimumab marks a watershed moment in lupus therapy. Clinical trials conducted by the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) demonstrated the drug’s efficacy in reducing disease activity scores and slowing the progression of lupus nephritis. The drug’s mechanism—blocking BAFF—highlights the critical role of B cells in lupus pathogenesis. In fact, a 2023 review in Nature Reviews Rheumatology underscored that B‑cell–driven autoimmunity is a hallmark of SLE, offering a clear rationale for biologic therapies.
Beyond belimumab, other biologics such as anifrolumab (a type I interferon receptor antagonist) are under investigation. According to the New England Journal of Medicine, anifrolumab has shown promising results in phase III trials, especially for patients with high interferon signatures—a subset of lupus that traditionally responds poorly to conventional therapy.
Genomic studies have also begun to map the genetic architecture of lupus. Large genome‑wide association studies (GWAS) have identified over 100 susceptibility loci, many of which are involved in immune regulation pathways. These insights are feeding into precision medicine approaches, allowing clinicians to tailor treatment plans based on a patient’s genetic profile.
Advocacy and Support
While the science progresses, Maria’s personal journey remains a powerful testament to the importance of patient advocacy. She became an active member of the Lupus Foundation of America (LFA) and frequently volunteers at local “Lupus Walks,” a fundraiser that supports research and patient education. “The community is incredible,” she says. “It’s comforting to know you’re not alone.”
Her participation in the LFA’s patient advisory board has also led her to contribute to patient‑reported outcome measures (PROMs) used in clinical trials. By sharing her lived experience, Maria helps shape research questions that truly matter to patients.
The LFA’s website (https://www.lupus.org) offers a wealth of resources, from educational articles to a patient support hotline. For those seeking clinical information, the Mayo Clinic’s lupus page (https://www.mayoclinic.org/diseases-conditions/lupus/symptoms-causes/syc-20374673) provides an accessible overview of symptoms, diagnosis, and treatment options.
A Hopeful Future
Maria’s story illustrates the journey many lupus patients endure—from delayed diagnosis to the search for effective therapy. Yet it also showcases how scientific advances are translating into tangible benefits. The shift from broad‑spectrum immunosuppression to targeted biologics, coupled with genetic insights, promises a future where lupus can be managed more safely and effectively.
“It’s not just about treating flares,” Maria reflects. “It’s about giving people a chance to live their lives, not just survive them.”
For more on lupus research and clinical trials, the National Institutes of Health’s National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) offers a database of ongoing studies (https://clinicaltrials.gov). As researchers continue to unravel the disease’s complex immune pathways, stories like Maria’s serve as both a reminder of the challenges ahead and a beacon of hope for the many living with lupus worldwide.
Read the Full The Independent US Article at:
[ https://www.aol.com/news/woman-journey-lupus-reflects-science-172248707.html ]



