Gut Microbiome Linked to Alzheimer's Progression
Locales: California, New York, Florida, UNITED STATES




Phoenix, AZ & Los Angeles, CA - February 10, 2026 - A groundbreaking study published today in Nature Communications significantly expands our understanding of Alzheimer's disease, suggesting a far more prominent role for the gut microbiome than previously imagined. Researchers from Arizona State University (ASU) and the University of Southern California (USC) have identified specific bacterial metabolites in the bloodstream that correlate with increased amyloid plaque accumulation in the brain and accelerated cognitive decline, key hallmarks of Alzheimer's disease.
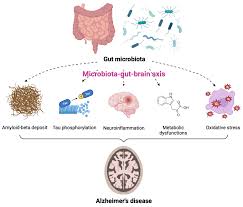
The study, analyzing data from over 1,000 participants in the long-running Alzheimer's Disease Neuroimaging Initiative (ADNI), builds upon a growing body of evidence establishing the 'gut-brain axis' - the bidirectional communication network between the gastrointestinal tract and the central nervous system. For years, scientists have suspected a link, but this research pinpoints specific microbial byproducts that appear to directly influence the disease process.
"We've moved beyond simply acknowledging that there's a connection to identifying what within the gut microbiome is potentially driving changes in the brain," explains Dr. Donald Ostrow, a professor in ASU's School of Nutritional Sciences and Methods Institute. "This isn't just about 'good' versus 'bad' bacteria; it's about the specific metabolites these bacteria produce and how those metabolites interact with the body's systems."
The researchers focused on identifying metabolites - small molecules produced by the metabolism of gut bacteria - circulating in the bloodstream. They discovered that elevated levels of certain metabolites, notably indoxyl sulfate, consistently appeared in participants exhibiting faster rates of cognitive decline and a greater buildup of amyloid plaques as revealed through advanced brain imaging. Indoxyl sulfate is a byproduct of tryptophan fermentation by gut bacteria. This suggests that the composition of an individual's gut microbiome can impact the production of these potentially harmful metabolites.
Dr. Ruobi Wang, an assistant professor at USC's Leonard Davis School of Gerontology and co-lead author of the study, emphasizes the complexity of the interaction. "The gut microbiome is incredibly diverse, and its influence extends far beyond digestion. It impacts immune function, inflammation, and even neurotransmitter production. What we're seeing with Alzheimer's is likely a disruption of this delicate balance, leading to an increase in pro-inflammatory metabolites and a decrease in beneficial compounds."
Implications for Prevention and Treatment
While the study confirms a strong correlation, researchers are careful to note that it doesn't establish definitive causation. "We need to prove that these metabolites are causing the changes in the brain, not just being associated with them," Dr. Ostrow clarifies. "That's the focus of our next phase of research."
However, the findings open up exciting new avenues for potential therapeutic interventions. If modifying the gut microbiome can indeed influence Alzheimer's progression, it suggests a relatively accessible and potentially preventative strategy. Researchers are exploring several possibilities, including:
- Dietary Interventions: Specific diets designed to promote a healthy gut microbiome - rich in fiber, prebiotics, and probiotics - could potentially reduce the production of harmful metabolites and support cognitive health. Personalized nutrition plans, tailored to an individual's microbiome profile, are also being investigated.
- Probiotic and Prebiotic Therapies: Supplementing with specific strains of probiotics (beneficial bacteria) or prebiotics (foods that feed beneficial bacteria) might help to reshape the gut microbiome and improve its functionality. However, identifying the right strains for Alzheimer's prevention is a key challenge.
- Fecal Microbiota Transplantation (FMT): Although more invasive, FMT - transferring fecal matter from a healthy donor to a recipient - is being considered as a potential, albeit long-term, therapeutic option for restoring a balanced gut microbiome.
- Metabolite Targeted Therapies: Direct intervention with specific metabolites through pharmaceutical approaches to reduce their concentration in the bloodstream, or to counteract their effects on brain tissue.
The ADNI cohort continues to provide crucial data, and the ASU/USC team is currently conducting follow-up studies to investigate the causal links between gut metabolites and Alzheimer's pathology. They are also exploring the potential for early detection - could gut microbiome analysis serve as a biomarker for individuals at high risk of developing the disease?
"This research is truly transformative," concludes Dr. Ostrow. "For decades, Alzheimer's research has focused primarily on the brain. Now, we're realizing that the answer may lie, at least in part, in the trillions of microorganisms living within us. It's a paradigm shift that could revolutionize our approach to preventing and treating this devastating disease."
Read the Full The Messenger Article at:
[ https://www.the-messenger.com/lifestyles/health/article_ae5bab0f-42aa-59f4-a2dd-824cd588948c.html ]











